|
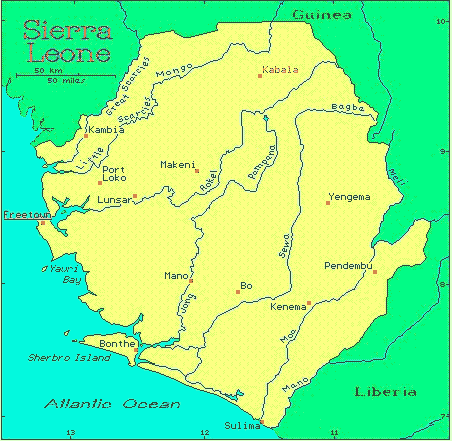
Yesterday, Friday, I heard from Claire again. We skyped for about 40 minutes, taking advantage of a fleeting episode of on-again, off-again electricity and WFI in the building where she was staying. Anyway, Claire and her Partners In Health team left Freetown, Sierra Leone, on Wednesday for the Ebola treatment unit in Port Loko, a rural area about 2 hours northeast of Freetown. On the way to Port Loko they passed through many checkpoints, mostly made of wood and rope, and they were stopped by police and soldiers for for a health screening at each town they entered. Upon their arrival in Port Loko some team members were assigned to a tent city set up by the Danish military while others, Claire among them, were assigned to an all-pink night club and hotel called The Sugar Sharg closed by the Ebola epidemic and now used as accommodations for medical staff. The view of the town of Port Loko from Claire's hotel. She said there are sheep and goats crossing the road at all times. During our Skype session Claire walked around with her computer to show me her accommodations: her bright-pink hotel room and bed canopied with mosquito netting and her "shower", i.e. the two buckets she fills with well water from a pump out in the court yard then hauls back into the bathroom, then standing over a drain in the floor, scoops up water from the buckets and dumps it on herself. Ironically, the Danish tent city has hot water, showers, electricity and WFI 24/7, though the residents must leave their tents to get to the bathroom. To which I responded, "Eh, like on the Camino sometimes." (See Tighten Your Boots", my daily blog of Tom's and my hike over the mountains of the Camino de Santiago de Compostela in Spain last year). After the tour of her room Claire walked outside with her computer to show me around the grounds a bit. She ran into a couple staff members, Eliska, the woman who runs the hotel and Muhammad, one of the two hotel security guards (both named Muhammad). Claire introduced us via Skype. Eliska, a nice-looking middle-aged lady, was very friendly and gracious and promised to take good care of Claire. While Eliska spoke English, the official language of Sierra Leone, Muhammad spoke only Krio, the country's native tongue, a mix of English, French, Portugese, and the African Yoruba an Igbo languages. Still Muhammed, dressed in a white tee shirt, jeans, and a red baseball cap, was friendly and showed me the hotel's well and water pump, and gave a demonstration on how the pump worked. They were nice people. How amazing that people from opposite sides of the world can connect through a video screen. Claire also showed me several pairs of scrubs - what the doctors and nurses wear under their Ebola hazmat suits - washed and hung out to dry on the barbed wire atop the hotel wall. After my tour Claire and I talked a while longer. She's now had two days working in the Ebola treatment unit. I asked her how it was wearing the Ebola gear and she said that the first time she put it on after 20 minutes she felt so hot and woozy that she was truly feared she was going to faint and wondered how in the world they'd ever get her out of her gear. However, she made it through the required hour in the suit and then the twenty minutes it took to get her out of the suit. She chalked her faintness up to dehydration - she drank 3 liters of rehydration salts after leaving the suit. Yesterday she made sure she was well-hydrated before putting on her gear and did better her second time. To prevent over-heating and dehydration a person can only be in the Ebola suit for an hour at a time - plus the twenty minutes it takes to be de-suited. A few hours later the person can then get suited up again and return to the Ebola treatment unit for another hour of work. The Partners In Health team members work along side local staff hired by PIH, hygienists who keep the unit clean, nurses, translators, and sprayers who follow the teams around spraying them and everything else with chlorine. PIH also hires Ebola survivors to help around the unit, especially to be with the sick children who are there without their parents. Claire said seeing the survivors caring for the children did her heart good. She said there were about 200 staff members working 'round the clock in the unit. As most of Serra Leoneans are Muslim, there is a prayer hutch on the unit where people stop during the day to pray. Claire also shared that she caught a glimpse of Partners In Health founder Paul Farmer. He stopped by the Ebola treatment unit and waved through the fence at the team all decked out in their Ebola gear. Claire said she stopped and waved back. Claire learned yesterday that today she will be moved to the Kono district, in the mountainous jungle region on the eastern border with Guinea where the country's diamond mines are located: There is no Ebola treatment unit yet in Kono, only community care clinics, some run by the Red Cross, that have been transporting their suspected Ebola patients to treatment units many hours away. Claire is not yet sure what to expect when she arrives.
Normally Partners In Health transports their team members from spot to spot by helicopter, but as today is Saturday and the next helicopter flight isn't until Monday Claire will be making the 11-hour trip by truck. She is most likely making that journey at this moment, as I write.
7 Comments
Jean Lewis
1/17/2015 08:14:06 am
Thank you Patti for keeping us informed. Our prayers and thoughts are with you Claire.
Reply
Patti
1/17/2015 11:04:46 am
Thank you, Jean.
Reply
molina
1/17/2015 11:13:35 am
Patti, all the while reading your posts, I share your pride and worry for your girl...praying for Claire and her team...keep on keeping us posted. God bless!
Reply
Patti
1/17/2015 12:16:54 pm
Heartfelt thanks, Molina.
Reply
Steve Liszkay
1/17/2015 08:35:37 pm
Patti - thanks for taking time to share your blog. It is fantastic. We hope for Claire's safe return.
Reply
Romaine
1/17/2015 11:17:35 pm
Thanks for the update on Claire - I think of her everyday and say a prayer that she is kept safe.
Reply
9/11/2017 01:17:26 pm
Trying to contact Steve liszkay. Please give him my number thanks coach borowy
Reply
Leave a Reply. |
"Tropical Depression"
by Patti Liszkay Buy it on Amazon: https://www.amazon.com/dp/B0BTPN7NYY "Equal And Opposite Reactions"
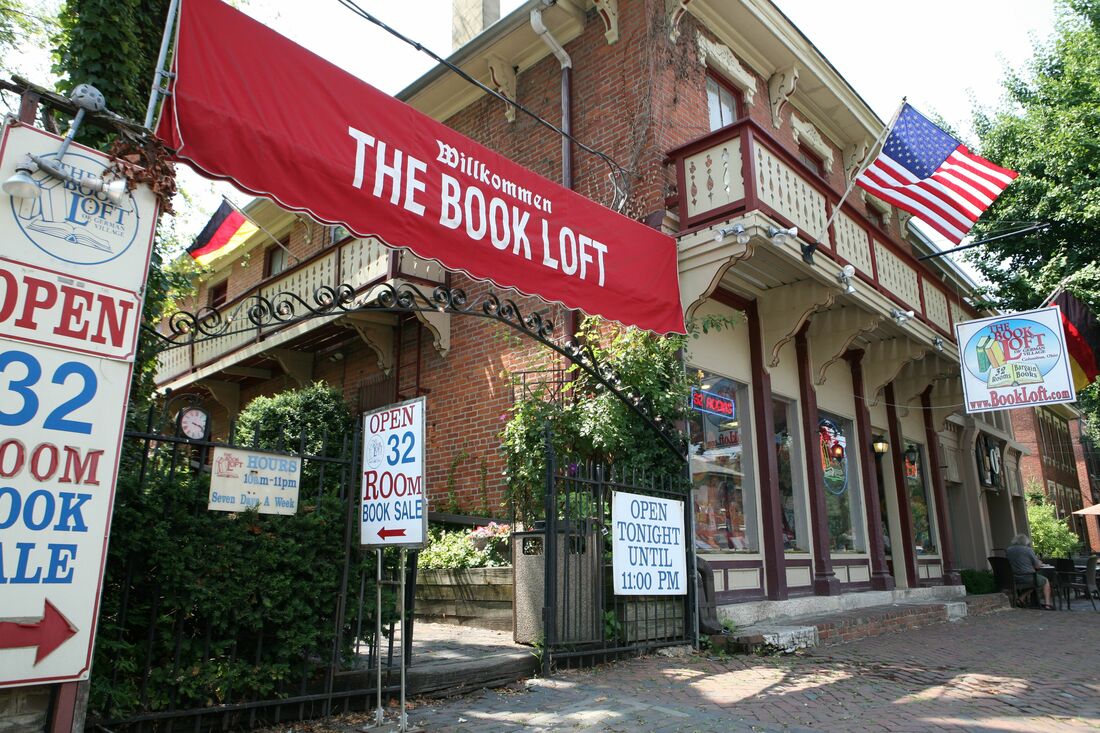
by Patti Liszkay Buy it on Amazon: http://amzn.to/2xvcgRa or from The Book Loft of German Village, Columbus, Ohio Or check it out at the Columbus Metropolitan Library
Archives
July 2024
I am a traveler just visiting this planet and reporting various and sundry observations,
hopefully of interest to my fellow travelers. Categories |


 RSS Feed
RSS Feed